At Wemos we believe in evidence-based advocacy. This also means keeping in touch with people who work on the ground and hearing their stories. During the 70th World Health Assembly in May 2017, Paul Nedermeijer and I had the opportunity to work with the People’s Health Movement (PHM) and the WHO Watch team. Among the group was Godfrey Philimon, a highly motivated Tanzanian public health advocate. I interviewed him about his perspectives on the human resources for health situation in Tanzania.
Godfrey Philimon works as a country coordinator for the PHM in Tanzania. PHM’s aim is to make the right to health real for Tanzanians. Godfrey Philimon volunteers as a country coordinator for PHM in Tanzania. Godfrey’s work for the PHM is voluntary; for a living, Godfrey is a farmer in a village five kilometers from Dar Es Salaam, in fruits and poultry. He holds a Bachelor of Arts in Political Science and Public Administration. After attending the classes from the international people’s health university program ‘The struggle for health’, he decided to pursue a career in Public Health and to build a PHM circle in Tanzania.
“I am very happy with my career and feel like public health is in my blood right now”
Human resources for health in Tanzania
According to Godfrey, a lack of health workers is one of the main problems with human resources for health in Tanzania. There are merely 5.2 clinical health workers per 10,000 people, one fifth of the ratio recommended by the World Health Organization – way too few for a strong health system. Poor working conditions and the lack of resources and equipment are just two of the underlying reasons. Godfrey says that key stakeholders – including patients – rarely address this situation.
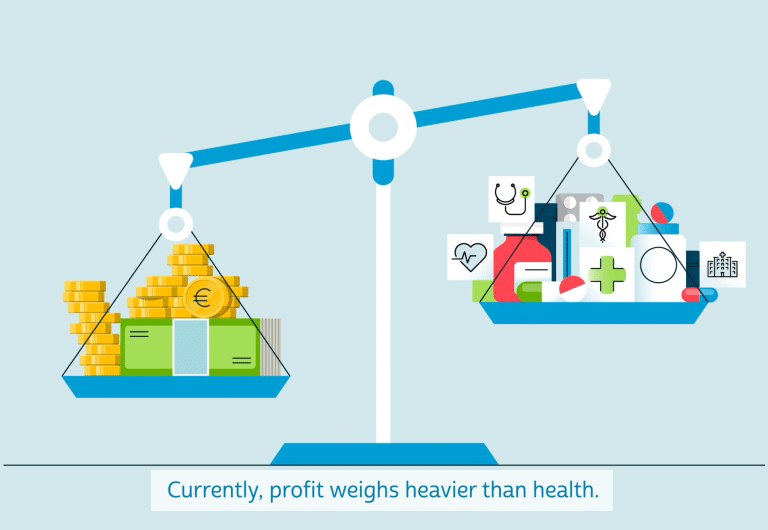
Furthermore, health professionals are being educated but not absorbed into the public health system. ‘Many are not employed due to governmental financial hardship’, he says. There has been too little attention for human resources for health by big donors and the government. He says that ‘the most critical factor driving health system performance, the health worker, has been neglected and overlooked for too long’. There is more money for medicines, but human resources for health remain underfunded. Godfrey stresses the need for advocacy for more financial support from donors to enable countries to mobilize the human resources they need.
Brain drain
The current lack of financing has led to brain drain, with a shortage mainly in rural areas, where the majority of the Tanzanian people live. Exact numbers are hard to find, because there are no tools to monitor health professionals’ domestic and international mobility. Due to poor living conditions in rural areas, health workers prefer to live in the city, and a lack of jobs in the national health system has pushed health workers to find alternative jobs. Educated health workers then move to the cities, private sector, neighboring countries or to other parts of the world, where there are other factors pulling them. This leaves particularly rural areas without the health workforce they dreadfully need.
“This movement of medical professionals leaves the sending country not only with a shortage of medical professionals, but leads to higher morbidity and mortality”
Global collaboration
At Wemos we believe that strengthening members of civil society at grass-root level is important to enable change. Godfrey argues that ‘the WHO might provide good support to these countries, but if these governments are not formulating good strategies, policies and frameworks which reflect health needs of their citizens, nothing will be achieved’. This is vitally important because, in his view: ‘There are health challenges which need to be advocated at country level and others at global level separately. When health advocates globally collaborate, we are much more effective.’